Introduction
Peripheral nerve blocks are gaining widespread popularity for perioperative pain management because of their specific advantages over general anesthesia and central neuraxial anesthesia.
Pain relief with PNB avoids side effects such as somnolence, nausea and vomiting, hemodynamic instability and voiding difficulty inherent to general and central neuraxial anesthesia.
Patients who undergo surgery under PNB can bypass phase I recovery room and frequently be discharged expeditiously following ambulatory surgery.
Patients with unstable cardiovascular disease can undergo surgery under PNB without significant hemodynamic changes.
Patients who have abnormalities in hemostasis or infection which contraindicate use of central neuraxial block can be candidates for surgery under PNB.
A substantial savings in operating room turnover time can occur if PNB is done outside the operating room. If the patient has a functioning block preoperatively there is no induction or emergence time. Patients with a PNB can frequently position themselves.
When used as part of a combined general regional technique, PNB facilitates lighter planes of anesthesia, avoiding the use of opioids and allowing a quick emergence and recovery.
In order to carry out a regional block safely and effectively, the anesthesiologist must be proficient in the following:
Anatomy
Have knowledge of the neural elements to be blocked, their relationship to muscular, vascular and other anatomic structures and their ultimate motor and sensory innervation. Knowledge of the innervation will provide guidance to select the most suitable technique for a particular surgical procedure. The bony, vascular, muscular and fascial relationships will serve as landmarks to guide the needle to the appropriate site, thus improving the success of the block and minimizing side effects and complications.
Pharmacology
Knowledge of local anesthetic pharmacology will assist in the selection of the most appropriate local anesthetic drug and dosage. The anesthesiologist must also be familiar with the clinical pharmacokinetics i.e. pattern of onset of and recovery of the nerve block. This allows an assessment of the clinical efficacy of the block with respect to operative anesthesia and approximate duration of postoperative analgesia after a particular local anesthetic drug has been injected.
Complications and side effects
Knowledge of the possible complications and the errors in the technique will help in preventing the complication and also in managing them effectively in case they do occur. Knowledge of the possible side effect which could occur from blockade of the other neural elements in the vicinity such as phrenic nerve, recurrent laryngeal nerve and the sympathetic nerves will help in patient education as well as in assessing the contraindication to the technique.
Local anesthetics: Clinical pharmacology, drug selection and toxicity
To select an appropriate local anesthetic drug for a specific clinical situation, one should be familiar with the clinical pharmacology of the local anesthetic drugs and adjuvants.
Local anesthetics exert their effect either by inhibiting the excitatory process in the nerve endings or in the nerve fibers. The following sequence of events is generally accepted as the mechanism of action of local anesthetic agents:
- Binding of the local anesthetic moiety to the receptor sites in the nerve membrane.
- Reduction in sodium permeability
- Decrease in the rate of depolarization
- Failure to achieve threshold potential
- Lack of development of propagated action potential
- Conduction blockade
The pharmacological activity of local anesthetic agents is influenced by their chemical structure, lipid solubility, protein binding, pKa.
Chemical Structure
Based on their chemical structure local anesthetics can be grouped into:
- Aminoesters – Procaine, cocaine, tetracaine, choroprocaine. Aminoesters have an ester linkage between the benzene ring and the intermediate chain. These are hydrolyzed in the plasma by pseudocholinesterase. One of the primary metabolites of ester compounds is paraminobenzoic acid. Paba has known allergic potential.
- Aminoamides – Lidocaine, mepivacaine, bupivacaine, ropivacaine. Aminoamides have an amide link between the benzene ring and intermediate chain. These are degraded in the liver by microsomal enzymes. The amide drugs are not metabolized to paraaminobenzoic acid and rarely produce allergic reactions. Multidose vials of amide local anesthetic may contain methylparaben (MPF should always be used for regional anesthesia) which is a paraaminobenzoic acid derivative with allergic potential.
Lipid Solubility
Lipid solubility is the primary determinant of intrinsic anesthetic potency. Potency increases as a function of lipid solubility until a blood/lipid partition coefficient of 4 is reached. Further increases in lipid solubility do not cause a further increase in the local anesthetic potency. Based on the lipid solubility and potency, local anesthetic drugs can be divided into 3 groups:
Low lipid solubility/potency: Lipid partition coefficient < 1. These drugs must be administered in high concentrations (2 to 3 %) to achieve effective neural blockade. Local anesthetic drugs in this category include procaine and chloroprocaine.
Intermediate lipid solubility/potency: Lipid partition coefficient 1-3. These drugs may be in concentrations of 1 to 2%. Local anesthetic drugs in this category include lidocaine, mepivacaine, and prilocaine.
High lipid solubility/potency: Lipid partition coefficient >4. These drugs are clinically effective at low concentrations <1%. Local anesthetic drugs in this category include tetracaine, bupivacaine, and ropivacaine.
Protein Binding
Addition of larger chemical radicals to the amine or aromatic end of a local anesthetic compound increases its binding to protein, which is a determinant of local anesthetic duration. Protein binding of commonly used local anesthetics is:
Bupivacaine-------------------------95%
Tetracaine---------------------------95%
Ropivacaine-------------------------94%
Mepivacaine------------------------74%
Lidocaine----------------------------65%
Procaine-------------------------------6%
PKa
Pka is the pH at which ionized and unionized fractions of a substance are present in an equal amount. The onset of local anesthetic effect will be determined by the total amount of unionized fraction of the local anesthetic agent because the unionized fraction primarily diffuses across the nerve membrane. The percentage of local anesthetic, which is present in the unionized form (cation or base) when injected into the tissue at (pH 7.4) is inversely proportional to the pKa of the agent. As the pH of the local anesthetic solution goes down, the unionized fraction will decrease when the pH increases the unionized fraction increases. There is a correlation between the onset of the block and the pKa of local anesthetic drug. The drugs with pKa of 7.6-7.8 ( lidocaine, mepivacaine, prilocaine) have a more rapid onset of action than do bupivacaine and tetracaine which have a pKa of 8.1 and 8.6 respectively. At the body pH (7.4), 35 % of lidocaine exists in unionized base form and only 5 % of bupivacaine exists in unionized base form.
Adjuvant Drugs
These drugs can reduce the onset time, prolong the duration, increase the density and reduce dosages of the commonly used local anesthetics.
- Epinephrine- Prolongs duration by vasoconstriction and slowed absorption. Duration can be increased by 30-50%. Peak plasma concentrations can also be reduced by 50%. Can also be a marker for intravascular injection—tachycardia.
- Clonidine- Prolongs duration of local anesthetics by synergistic alpha-2 effects. Lesser or no prolongation with Bupivacaine and Ropicacaine but can prolong Mepivacaine-Lidocaine by 40-400% with 100 micrograms. Larger doses are not additive and cause more side effects.
Upper Extremity Blocks
The plexus of nerves innervating the upper extremity is contained in a fascial sheath, which is surrounded by reliable anatomic landmarks. This allows an injection of local anesthetic to reliably block the sensory and motor innervation to the upper extremity with two exceptions—
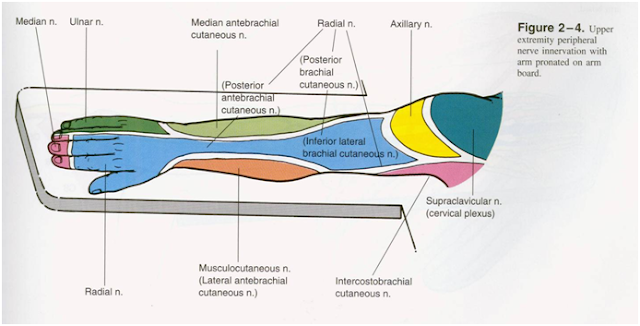
Areas of the upper extremity with cervical plexus innervation. The sensation of the skin overlying the shoulder is supplied by the nerve roots C3 and C4 of the cervical plexus. These nerve roots lie superior to the most cephalad aspect of the brachial plexus. Interscalene blocks done with large volume of local anesthetic (35-40ml) may block these nerve roots as well in the vast majority of cases. The surgical procedures where C3 and C4 blocks are beneficial usually involve the clavicle.
Area of the upper extremity with intercosto-brachial (T2) innervation. The sensory innervation of the axilla and anterior shoulder is T2, which is also derived from outside the brachial plexus. A T2 block is required for shoulder surgery with anterior incisions (anterior stabilization for shoulder dislocation) and surgery involving the elbow and upper arm.
Innervation of the upper extremity
For convenience the branches of the brachial plexus which innervate the upper extremity can be divided into supraclavicular (branches from roots and trunks) and infraclavicular branches from the divisions, cords and nerves.
All the supraclavicular branches are motor with the exception of the suprascapular nerve, which provides sensation to the shoulder joint. Suprascapular branches supply the scalene muscles, serratus anterior via the long thoracic nerve, muscles of the upper back and contribute to the phrenic nerve.
The infraclavicular branches comprise all of the sensory and motor innervations to the upper extremity and are important to the anesthesiologist both from the point of view of technique (distribution of parasthesia, motor response if nerve stimulator is being used to locate the plexus) and extent of the block and identification of missed nerves.
Anatomic relations of the Brachial plexus
Knowledge of the anatomic structures, which surround the brachial plexus, will help in the location of the plexus as well as in the prevention of complications.
Perivascular compartment
This concept has promoted the single injection technique of the brachial plexus block. Clinically, proximal blocks behave as if there were a sheath surrounding the plexus. A single injection technique lends itself to a short onset and high success rate. However with a more distally placed block like an axillary block, a single injection technique is less reliable because of the individual peripheral nerves begin to diverge. To improve the success of an axillary block several strategies are used to improve proximal spread of local anesthetic- such as injecting high in the axilla, adduction of the arm and application of pressure distal to the injection.
Vascular relationship
There are no major vessels at the level of the roots except for vertebral vessels, which lie far medially and anterior to the plexus. A long needle directed horizontally in the interscalene space may get into the vertebral artery or vein. The needle can also get into the subarachnoid or epidural space via the intervetebral foramen. The trunks of the plexus also lie in close proximity to the subclavian artery, which separates them from the anterior scalene muscle. . This relationship must be born in mind when doing a subclavian perivascular approach is being used. Another anatomic fact is the significance that the inferior aspect of the trunk of the plexus may be trapped behind and under the artery. In this situation, there is probably a mechanical barrier to the spread of local anesthetic if it is placed high in the interscalene groove. So the most common elements of the brachial plexus missed with an interscalene approach are C8 and T1.
Blocks above the clavicle
Level of the roots – Interscalene brachial plexus block
Trunks – Subclavian perivascular brachial plexus block/ classical supraclavicular brachial plexus block
Blocks below the clavicle
Division/Cords – Infraclavicular brachial plexus block
Cords/Terminal nerves – Axillary brachial plexus block
Axillary Approach of the Brachial Plexus
The axillary block is the most commonly used approach to the brachial plexus since this approach is free of the risk of pneumothorax.
Position: The patient is placed supine with the arm abducted 90 degrees and flexion of the forearm with external rotation so that the forearm lies parallel to the long axis of the body. Hyperabduction will obliterate the axillary artery pulse in 80% of individuals because the artery is compressed between the head of the humerus and the pectoralis minor muscle.
Needle placement: The arterial pulse should be identified and followed as proximal as possible, ideally to the point where the pulse disappears beneath the pectoralis major. The artery is located between the index and middle fingers of the non-dominant hand. With light digital pressure the artery is fixed against the humeral head high in the axilla. A #22 gauge 1.5 cm B bevel needle is introduced slightly superior to the finger tip and advanced at about a 30 degree angle to the skin, tangential and parallel to the neurovascular bundle until one of the following 3 endpoints are met.
Slow needle placement until a parasthesia is obtained (Success rate 85-90%).
The transarterial approach: The needle is slowly advanced until bright red blood is obtained during continuous advancement. Once blood return is obtained, the needle should be advanced through the wall of the axillary artery until no additional blood can be aspirated. Once it has been verified by the aspiration that the needle tip lies posterior to the arterial wall (just 1-mm), the total anesthetic volume (40-50 ml) is injected in 5-ml increments posterior to the artery. Splitting the local anesthetic volume to deposit posterior and anterior reduces rather than increases the success rate of the block. The success of the block is related to the close proximity of the needle tip to the posterior wall of the artery (clinical sign to ensure this is aspiration of slight blood stained fluid during intermittent aspiration and injection). After approximately 20 ml of local anesthetic injection the needle can be withdrawn back though the artery and advances again through the posterior wall. This reconfirms that the needle tip is in close proximity to the posterior wall of the artery. Appropriately performed, the transarterial approach has nearly 100% success rate. A sharp needle (not a blunt tipped nerve stimulator needle) should be used for the transarterial technique.
Axillary block using a nerve stimulator – Using an insulated needle, connect the negative lead to the needle. Use low output current (.3-.5ma) at l sec twitch rate. Look for an appropriate motor response in the hand in the distribution of the ulnar, radial, or median nerves. Please note that motor response at the elbow (biceps twitch) indicates that stimulation of the musculocutaneous nerve, which is outside the sheath. The injection at the endpoint will result in the block of the musculocutaneous only.
Epinephrine 1:200,000 (5 mcg/ml) should be used in all perivascular blocks. Direct close attention to the ECG or pulse oximeter pulse tone to effectively identify intravascular injection. After injecting 40-45cc, a small volume of local anesthetic should be injected subcutaneously over the axillary artery to block the branches of the intercostobrachial and medial brachial cutaneous nerve.
Assessing the Success of the Axillary Block
If the onset of proximal motor block (loss of forearm extension; i.e. inability to point to the ceiling – radial nerve block) occurs within minutes of the injection, you can expect good surgical anesthesia in 20 minutes. Check the sensory distribution of the individual nerves to identify the unblocked nerves.
(Push, Pull, Pinch, Pinch)
Interscalene approach to the brachial plexus
This technique for brachial plexus anesthesia is used for surgical procedures of the upper arm and shoulder. This approach is specifically suited for shoulder surgery since it blocks the suprascapular nerve which supplies sensation to the shoulder joint.
Technique: The key to success is correct identification of the interscalene groove. The patient should be supine and asked to elevate the head, bringing the sternocleidomastoid muscle into prominence. The index and middle fingers are places behind the clavicular head of the sternocleidomastoid muscle and the patient is asked to relax and turn the head and onto the opposite side with the chin in the midclavicular line. Turning the neck too far laterally will make the scalene muscles difficult to palpate. The palpating fingers are moved medially behind the sternocleidomastoid to lie on the anterior scalene muscle. The palpating fingers are then rolled laterally until the groove between the anterior and middle scalene muscles is identified. Please note that the groove is wider distally, so keep the distal palpating finger in the groove just above the clavicle. Keep the middle finger firmly in the distal part of the groove and the palpating index finger at the level of C6 anterior to the external jugular vein. If there is difficulty in identifying the anterior scalene muscle, ask the patient to maximally inhale. This makes the anterior scalene muscle more prominent and its palpation easier. The needle is inserted in the into the interscalene groove at the level of C6 which can be identified by drawing a line from the crycoid cartilage to the interscalene groove. An additional landmark is the external jugular vein when visible crosses the interscalene groove at the level of C6. With both the index and middle fingers in the groove, a #22 gauge B-bevel needle is inserted at the level of C6 perpendicular to all planes mostly mesiad, but slightly caudad and posterior. . The appropriate needle placement should be 60 degrees from the sagittal plane. The needle is advanced until a parasthesia is elicited in the shoulder or there is a motor evoked response in the forearm at <0.5 mA or the transverse process is contacted. If bone is contacted then the needle tip should be withdrawn and redirected caudad until the appropriate motor response or parasthesia is obtained.
Please note that when a large volume of local anesthetic (35-40 ml) is injected especially in a thin patient, a visible swelling will appear above the clavicle defining the inferior portion of the supraclavicular brachial plexus. Due to the distance of the C8 and T1 nerve roots from the sight of injection, the ulnar nerve is frequently missed with the interscalene approach. Also, the intercostobrachial and brachial cutaneous nerves, which supply the axilla and medial aspect of the upper arm, will be missed.
Assessing the success of the Interscalene Block
Motor block precedes sensory block. Innervation to the shoulder flexors are the first blocked. If the patient cannot lift the shoulder of the table within 2-3 minutes of local anesthesia (even with 0.5% Bupivacaine) expect good surgical anesthesia for shoulder surgery within 20 minutes.
.
Infraclavicular brachial plexus block
Anatomy: The boundaries of the infraclavicular fossa are pectoralis major and minor muscles anteriorly, ribs medially, clavicle and coracoid process superiorly and humerus laterally. The plexus is approached in close proximity to the coracoid process.
 Technique: the patient is supine, the ipsilateral arm is abducted to a 90-degree angle and the patient’s head is turned to the opposite side.
Technique: the patient is supine, the ipsilateral arm is abducted to a 90-degree angle and the patient’s head is turned to the opposite side. The following landmarks are identified and marked –
Medial head of the clavicle
Acromion process – The most prominent structure on the superior aspect of the shoulder. Axillary artery – at the highest point in the axilla place a mark on the pectoralis major, Doppler can be used to mark the axillary artery along the infraclavicular area
Mark the midpoint of the clavicle between the Acromion and the sternal head of the clavicle.
Needle entry site is – 2.5 cm below the midpoint of the clavicle along the axillary artery.
The anesthesiologist stands at the patient’s side opposite to the one being blocked. The needle entry site is infiltrated with local anesthesia. A 10 cm insulated block needle is inserted at a 60 degree angle to the sagittal plane directed away from the rib cage towards the axilla. Pectoralis major contractions are observed at a depth of 1 – 3 cm. The plexus lies 3 – 7 cm deep. Since musculocutaneous and axillary nerves are outside the sheath, motor response of those two nerves (i.e. deltoid and biceps contractions) should not be accepted. If these two motor responses are obtained redirect the needle injection toward the apex of the axilla. The ideal motor evoked response is hand movement at (.3-.4)mA. Once ideal motor evoked response is obtained inject 40 – 50 ml of local anesthesia incrementally. If no motor response is encountered, progressive needle redirection to 80 degrees will yield an appropriate response.
Suprascapular Nerve Block
The suprascapular nerve provides sensory innervation to 70% of the shoulder joint. The suprascapular nerve supplies Superior and posteriosuperior regions of the shoulder joint capsule and variable portions of the overlying skin. Anteriorly and inferiorly the skin and joint capsule are supplied by the axillary nerve, upper and lower subscapular nerves. Suprascapular nerve blocks can be used for postop analgesia but not for operative anesthesia.
Technique: The patient should sit up and lean forward with the arms hanging loosely at the side. Draw a line along the length of the spine of the scapula. Palpate the acromion process at the edge of the spine of the scapula. At the point where the thicker acromion process fuses with the thinner spine of the scapula is marked. The skin is prepped. A 25 or 27 gauge needle is used to anesthetize the needle entry site at the marked point. An insulated block needle – (Stimuplex) 22g 2 inch (<70 kg) or 4 inch (>70 kg) is introduced through the marked point. The needle should contact bone at a depth of one inch. The needle is walked superiorly and medially until it slides off into the suprascapular notch. The needle should be advanced no more than 1 cm from the suprascapular notch because of the risk of pneumothorax. Stimulation of the suprascapular nerve causes contraction of the supraspinous and infraspinous muscles with abduction and external rotation of the arm. With the appropriate motor evoked response, inject 10 – 15 ml of local anesthesia.
Intravenous Regional Anesthesia (IVRA, Bier Block)
IVRA can be used for short surgical procedures on the extremities. IVRA involves an IV injection of local anesthetic mixture into an exsanguinated extremity that is vascularly isolated by a tourniquet. It is technically simple. High reliability (97-100%), ease of administration and safety are major advantages of this technique. IVRA is suitable for surgical procedures below the elbow in the upper extremity and below the knee in the lower extremity of less than 1-hour duration. The only drug specifically approved by the FDA for IVRA is Lidocaine 0.5% preservative-free. For upper extremity blocks, a volume of 40-50 ml is used and for the lower extremity blocks, a concentration of 0.25% with a volume of 100-125 ml is used. The purpose of using a high volume is to assure an adequate distribution of local anesthetic in the entire venous system of the exsanguinated extremity.
Technique of IVRA
Start an IV infusion in the uninvolved extremity for drug administration and hydration.
Apply the appropriate monitors; give supplemental oxygen and adequate sedation to make the patient comfortable. Check baseline SBP so that the appropriate tourniquet inflation pressure can be used (100 mm Hg higher than SBP).
Place a 20 or 22 G angiocath near the surgical site preferably in the dorsum of the hand. Do not place the angiocath near the site of the surgical incision.
Apply Webril gauze to the upper arm from armpit to elbow. This protects the skin and the ulnar nerve in the cubital tunnel.
Apply two separate tourniquets of the Webril. Place a 24-cm tourniquet proximally and 18-cm tourniquet distally on the upper arm. In obese patients with conical shaped upper arm, use a single large 30-cm tourniquet.
Elevate the extremity and exsanguinate with an Esmarch bandage from hand to distal tourniquet. While wrapping the arm be careful not to wrap the area over the angiocath. Compression of the angiocath hub beneath the Esmarch bandage can cause ulceration of the underlying skin.
Inflate the distal tourniquet to 250-mm Hg and then inflate the proximal tourniquet. Once the proximal tourniquet is inflated, deflate the distal tourniquet. Ensure that the inflation pressure is at least 100 mm Hg above the systolic pressure. In a hypertensive patient > 250 mm Hg may be needed. This is very important for maintaining a bloodless surgical field.
Remove the Esmarch bandage and check for presence of a radial pulse.
Place a tourniquet proximal to the angiocath on the forearm and inject the local anesthetic solution into the angiocath slowly.
Remove the angiocath and compress site for 2 – 3 minutes.
Tourniquet Pain
Tourniquet pain manifests itself in many forms: e.g. patient getting restless, vague complaints of aches and pains and pressure in the arm, tourniquet site, or in the shoulder. This may occur 20-30 minutes after the inflation of the proximal tourniquet. If you suspect that the patient is having tourniquet pain, inflate the distal cuff then deflate the proximal cuff. Always inform the surgeons before switching the tourniquets as they may be in the middle of a crucial maneuver and any tourniquet mishap may complicate their procedure. Supplemental analgesics and sedatives are also used to prevent and manage tourniquet pain.